What is my normal blood pressure? |

Should you aim for an even lower blood pressure goal?
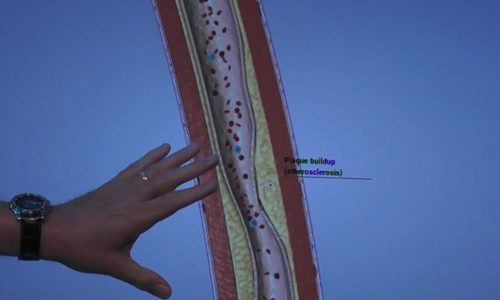
There is a hot debate going on right now between physician groups about blood pressure treatment. Specifically, when should we start prescribing blood-pressure lowering medications? When systolic blood pressure is greater than 140/90? Or perhaps we should begin when it’s as low as 130/80 if the patient has one additional risk factor? This is a very important question because we know that high blood pressure puts people at risk for strokes, kidney and heart disease, and even death. So what is the ideal blood pressure and should we give patients more drugs to achieve the goal?
In a bold move, The American Academy of Family Physicians (AAFP) did not endorse The American Heart Association (AHA) and American College of Cardiology’s (ACC) new guidelines to begin treatment at the lower pressure of 130/80. The AAFP represents the majority of family physicians in America (about 129,000 of them) while the ACC represents the majority of cardiologists (49,000 strong.)
According to the AHA, the lower treatment threshold would lead to 46 percent of the U.S. adult population being categorized as having hypertension. Using the previous threshold, that figure would be 32 percent of American adults.
Changing the definition of “high blood pressure” therefore, has the potential to add 42 million Americans to the treatment pool for this condition. And before we do that, we should have pretty strong evidence that this will help more than harm, right?
The problem is that although there is evidence of benefit (decreased damage to the heart when hypertension is treated early) the potential harms are less clear. And this is why the AAFP is not endorsing the move, recommending that treatment be a shared decision between patients and their physicians.
As a rehab physician, I treat patients who have injured themselves after falling down. I have found that over-medication is a very common contributor to falls, especially as we age. Patients can feel weak or faint when their blood pressure gets too low, and sometimes well-meaning efforts to keep blood pressure in an ideal range results in an over-shoot. Often times, my patients are also on blood thinners (such as warfarin, aspirin, or newer drugs like dabigitran, apixaban, and rivaroxaban) when they fall, and can bleed fairly profusely, even inside the brain, resulting in very serious and life-threatening damage.
So before you decide to take medicines (or more medicines) for your blood pressure, here are a few things to ponder:
- Do you really have high blood pressure? Blood pressure measurement in the doctor’s office (when you may feel nervous) sometimes overestimates actual blood pressure. Check your blood pressure on several different days when you’re very relaxed at home. Take those results to your doctor to give him or her a sense of your true resting blood pressure.
- Can you sufficiently reduce your blood pressure through “natural” methods? Weight loss, regular exercise, and reduced salt intake may reduce your blood pressure enough not to need (more) medications. Weight loss of as little as 10 pounds is enough to make a clinically significant difference in blood pressure.
- Are you at higher-than-average risk for falling? Do you have neuropathy (decreased feeling in your feet), weakness or clumsiness of any kind? Any history of falling? A risky job that makes falling more likely?
- Are you taking blood thinners? This greatly increases the potential harm to your body if you do fall down (or are knocked down by a pet) or have another unanticipated event.
Besides the risk of falling, very low blood pressure can occur when you are taking medicine and also become dehydrated or sick. In extreme cases, this combination can be fatal.
So although it’s important to manage high blood pressure, over-managing it is not safe. Please talk to your doctor about whether or not you need more medication. Because in my opinion, less is often more!
References
https://www.mayoclinic.org/diseases-conditions/high-blood-pressure/in-depth/high-blood-pressure/art-20045868
http://www.acc.org/guidelines/hubs/high-blood-pressure
http://www.acc.org/latest-in-cardiology/articles/2017/11/08/11/47/mon-5pm-bp-guideline-aha-2017
https://www.aafp.org/news/health-of-the-public/20171212notendorseaha-accgdlne.html?cmpid=em_AP_20171213
https://www.nhlbi.nih.gov/files/docs/public/heart/hbp_low.pdf
If you have any more questions just Ask Hanna, our health advisors are here to help.
Image: ©Shutterstock / fizkes